Stroke and Occupational Therapy
Two Common Types of Stroke

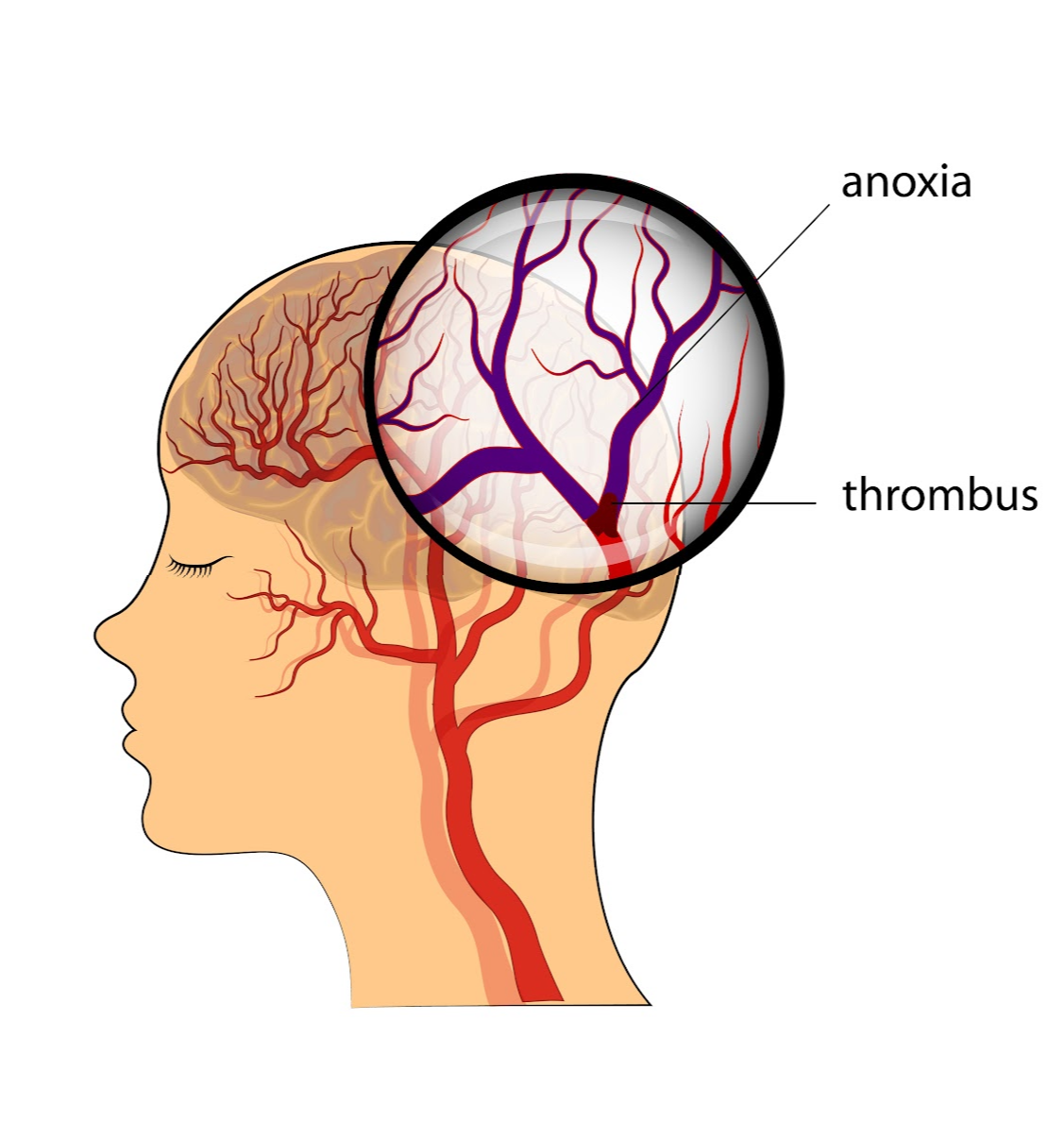
Hemorrhagic Stroke
- Occurs when a blood vessel ruptures or leaks, most commonly because of hypertension bleeds, malformed blood vessels or veins, aneurysms (blood vessel weakness), or it may be spontaneous.
- Causes excess blood to come in contact with other brain tissues which is an irritant
- Can cause the skull to fill up with ruptured blood which then squeezes brain tissues and causing significant damage and pressure.
Ischemic Stroke
Embolic Stroke – This occurs when a clot breaks free and travels through a vessel before causing a blockage. This traveling clot, called an embolus, May originate from vascular plaques and deep vein thrombosis (DVT)
Thrombic Stroke – occurs as a result of buildup inside of the blood vessel, usually through atherosclerotic disease. This buildup occludes (blocks) the artery.
Potential for Recovery after Stroke
This video demonstrates interventions for right-sided stroke in a left-side dominant individual. It showcases the use of mirror therapy to activate mirror neurons and promote motor control pathways. The importance of patient handling and positioning to prevent maladaptive compensation is highlighted. Clonus at the end range of active motion in stroke patients is discussed. Grading activity based on client skill is emphasized for improvement. Bilateral training and motor overflow techniques are used to enhance motor tasks on both sides of the body. The patient in the video achieved functional use of tone, self-correction of posture, and fluid movement patterns.
What is synergy?
After a stroke, flexor synergy patterns typically affect the arm, causing involuntary movements like shoulder flexion, elbow bending, and wrist/finger flexion, making it difficult to reach or straighten the arm. Extensor synergy patterns commonly impact the leg, leading to hip extension, knee straightening, and foot pointing, which can hinder walking. These involuntary patterns limit functional movement, so occupational therapy focuses on breaking these synergies by promoting controlled, isolated movements to improve independence in daily activities.
Download Synergy ResourceSymptoms and Other Effects
How does stroke impact the body?
In occupational therapy, understanding which brain arteries supply specific regions helps practitioners identify which functions may be affected by a stroke. Different arteries control areas responsible for movement, speech, vision, or coordination. By knowing which artery was impacted, your occupational therapist can tailor your treatment plan to address the specific symptoms you’re experiencing—whether it's difficulty with motor skills, speech, or balance—helping you regain independence more effectively.

Circle of Willis
Anterior Cerebral Artery (MCA)
Middle Cerebral Artery (ACA)
Posterior Cerebral Artery (PCA)
Basilar Artery
Vertebral Artery
Anterior Inferior Cerebellar Artery (AICA)
Posterior Inferior Cerebellar Artery (PICA)

Functions and
Brain Regions
A colorful quick reference to laminate for the clinic and functions associated with injury to client.

Symptoms by
Brain Region
A colorful quick reference to laminate for the clinic and explain symptoms to client.

ABI Symptoms
An 11-page quick reference for understanding symptoms associated with ABI.
Examination and Evaluation
Body Functions Impacted by Stroke
When a stroke occurs, it disrupts the blood supply to specific areas of the brain, leading to damage that affects various body functions. Depending on the part of the brain that is injured, different functions can be impacted, such as movement, speech, balance, and vision. These changes can affect your ability to perform everyday tasks, from dressing and eating to walking and communicating. Understanding which body functions are impacted helps guide targeted rehabilitation, enabling your recovery to focus on the areas most affected by the stroke.
Download a Resource of Stroke Symptoms
What is the difference between examination and evaluation?
Examination: Gather information through objective measures, clinical observation, interviews, and chart review.
Evaluation: Analyze and Interpret the findings obtained during your examination.
Download Occupational Profile Interview TemplateHelpful Objective Measure Links
Controlled Oral Word Association Test
Kurtzke Expanded Disability Status Scale (EDSS)
The Health Assessment Questionnaire **
Lower Extremity Functional Scale
Stereognosis
Dull Sharp Test or Somatosensory status
Examination
Diagnosis
-
When where they diagnosed?
-
Who diagnosed them?
-
What prompted them to seek out a diagnosis?
-
What other conditions do they have? (Lupus, fibromyalgia, Arthritis, CT tissue disease, etc) – This will impact your intervention approach!
-
What symptoms are most affecting them right now in their quality of life
-
What are they most nervous about with their diagnosis?
-
What do they know about their diagnosis and what questions do they have?
-
What would they like to do to address their symptoms?
-
What did the doctor say about their status and when is their next follow-up appointment?
-
Have the received any type of injections for spasticity to date? When? When are there next ones scheduled? (This will be based on place setting).
Occupational Profile
-
Social support, living situation, community activity, activities or occupations being impacted, life roles and how they have been impacted.
-
Environmental and participation barriers in ADLs, IALDs, and other 7 domains of occupation.
-
Health management and how diagnosis and underlying conditions are impacting occupations, medication management
-
Determine if patient is a good historian or will you need to include a caregiver interview?
Considerations during assessment preparation
There are things to consider that may be worth addressing during the initial “information gathering” time with your patient. These are some of them:
-
Coping strategies for long-term chronic disease management
-
Psychosocial and Perception-based deficits including locus of control, altered participation in life activities, how capable they believe themselves to be, body image, and fear of pain
-
Do they know how to manage their diagnosis along with their primary diagnosis (if applicable)
Writing the Assessment Section
In the assessment you will use clinical insight and current research of diagnosis and therapeutic potential to interpret the subjective information you collected and the outcomes of the assessments you conducted. You must include why restorative services are warranted and what the occupational therapy plan of care will address.
Include the necessity for caregiver training and support throughout the progression of the illness as new barriers will present themselves regularly throughout the continuum which will ultimately impact the carer’s ability to fulfill their role unless OT services are recommended
In your assessment, explain to the reader why OT services should be reimbursed instead of another profession, a non-skilled worker, or self-help resources from online.
Some other things to include in your assessment section:
-
Type of stroke, part of the brain impacted, expected symptoms to be further addressed in future sessions
-
Therapeutic potential and rationale
-
Potential barriers to success
-
Social and Environmental supports for patient success
-
Initial research-supported interpretations of your findings
Developing Your Plan
This is the same for all diagnoses.
-
How long should your plan of care be?
-
What is the frequency and level of intensity?
-
Based on the data you collected (subjective and objective) and your clinical interpretation (assessment)
-
What will your continuum look like?
Hint: This is where you use research according to the goals you are working toward to understand how long it will take to get similar results! Maybe your goals aren’t exactly listed and defined in the research – no worries! This is common because OT combines many different models of practice and frames of reference within social and medical models of medicine!
Use activity analysis to break down the mechanisms of the activity demands and clinical barriers – how do similar research studies approach these elements? This is how you begin creating a plan of care and treatment continuum for your client!
Download Treatment Plan Communication TemplateInterventions for Stroke
Physical Interventions
Download the "Principles of Neurorehabilitation after Stroke" Handout-
Use Meaningful tasks [ this does not mean occupation-specific tasks, it means ensure that your patient has achieved buy-in with your approach]
-
Strengthening and resistive exercise [if patient has adequate excursion of joint volitionally without compensations]
-
Constraint-induced movement therapy when appropriate
-
Mirror Therapy when appropriate
-
Bilateral training and weight bearing during functional tasks
-
Cognitive remedial therapy
-
Action-observation training and mental imagery as home programs
-
Train the client how to perform self-range of motion exercises and instructing them not to go beyond 90 degrees of shoulder flexion or abduction if inadequate scapulohumeral rhythm is noted
-
Encourage use of the affected upper extremity in all daily tasks
Main concerns to watch
-
Shoulder subluxation
-
Scapular dysfunction
-
Shoulder hiking of the affected upper extremity with contralateral trunk flexion to perform functional tasks
What not to do
-
Use a pulley for range of motion in the presence of shoulder/scapula dysfunction
-
Wrap a hemiparetic limb on an arm bike without proximal support and use the non-affected limb to move it
Spasticity
One of the hallmark symptoms of stoke is spasticity. This can look and heal differently in every patient you see. The path of motor learning after stroke is filled with ups and downs, but the occupational therapy practitioner can help someone experiencing spasticity in numerous ways.
Download Spasticity ResourcePsychosocial Interventions
Download 'Self-Administered Comorbid Questionnaire'-
Post-stroke anxiety – an overwhelming sense of worry and fear.
-
Interventions for Activity of Daily Living and Instrumental Activities of Daily Living Impairments
Education
-
Disease information, prognosis, and process
-
Potential symptoms and solutions
-
Joint protection (especially if patient is experiencing subluxation or ‘scapular winging’
-
Energy Conservation training across multiple contexts
-
Task simplification
-
Fatigue management
-
Home Exercise Program
Occupational Interventions
Download a list of Adaptive Stategies and Supplies for One-armed lifestyle supportSelf-Feeding (Positioning)
-
Obtaining an upright seated position
-
Placement of food and objects
-
body mechanics to bring food from plate to table
-
Temporary compensation or adaptation to achieve independence in self feeding prior to full recovery
Postures and Techniques
-
Chin tuck is used to initiate a swallow in a system potentially protect the airway by constricting it. It is thought that a chin tuck position May decrease aspiration in some, but should not be recommended to the exclusion of further testing
-
Head turn is when the head is rotated toward the weaker side in conjunction with a chin tuck can also decrease aspiration
-
Mendelsohn maneuver – encourage the client to push tongue into hard palate while swallowing which helps by opening the pathway for a swallow
Exercises and Strengthening
-
ROM of the jaw, tongue, and cheek, and oral motor tasks such as blowing air into a balloon and sucking through a straw.
-
Lip and tongue exercises have proven useful with client after a stroke to increase strength and coordination
Adaptive Equipment : Built-up utensils, contrasted items for visual perceptual deficits, Universal Cuff for decreased fine motor recruitment and mobility, kitchen equipment that promotes independence in meal preparation.
Dressing
Remediate structures, functions, and functional movement patterns – Therapeutic Exercise and Neuromuscular Re-education for postural mm strength and endurance as well as sitting/standing dynamic balance prior to offering suggestions for occupation-specific execution without assistance.
Upper Body Dressing with hemi-dressing techniques
-
Magnetic zipper to assist with closure
-
Button hook
Lower Body Dressing
-
Magnetic pant closures
-
Using Velcro for closing pants
-
Hemi-dressing techniques
-
Dressing Stick
Environmental Interventions
Home modifications/AE – if the client communicates environmental barriers
-
Avoid DME as long as possible with physical-based plans of care. Never jump right to DME if not necessary
-
Continuously introduce adaptive mobility techniques for potential ADLs or IADL affected by primary symptoms – This should happen WHILE you are working to improve the actual symptoms!!!! This is not INSTEAD of working with the physical restorative plan of care! This is a supplement! A partnership!
Life Space Questionnaire with Life Space education and handout