Amyotrophic Lateral Sclerosis
"Our role isn’t to fix ALS—it’s to support function, preserve dignity, and walk alongside those who face it."
CLICK HERE to Ask a Question [Easy Navigation]

Clinician Guide
This clinician resource is written with simple text to equip the practitioner with enough information to get them started when working with someone diagnosed with PD.

Patient Guide
This visually appealing packet of handouts is designed to improve understanding of PD and equip someone with strategies to maintain wellness.
Evaluation
Things to know before and during your evaluation.
Click Here for General Evaluation and Examination Information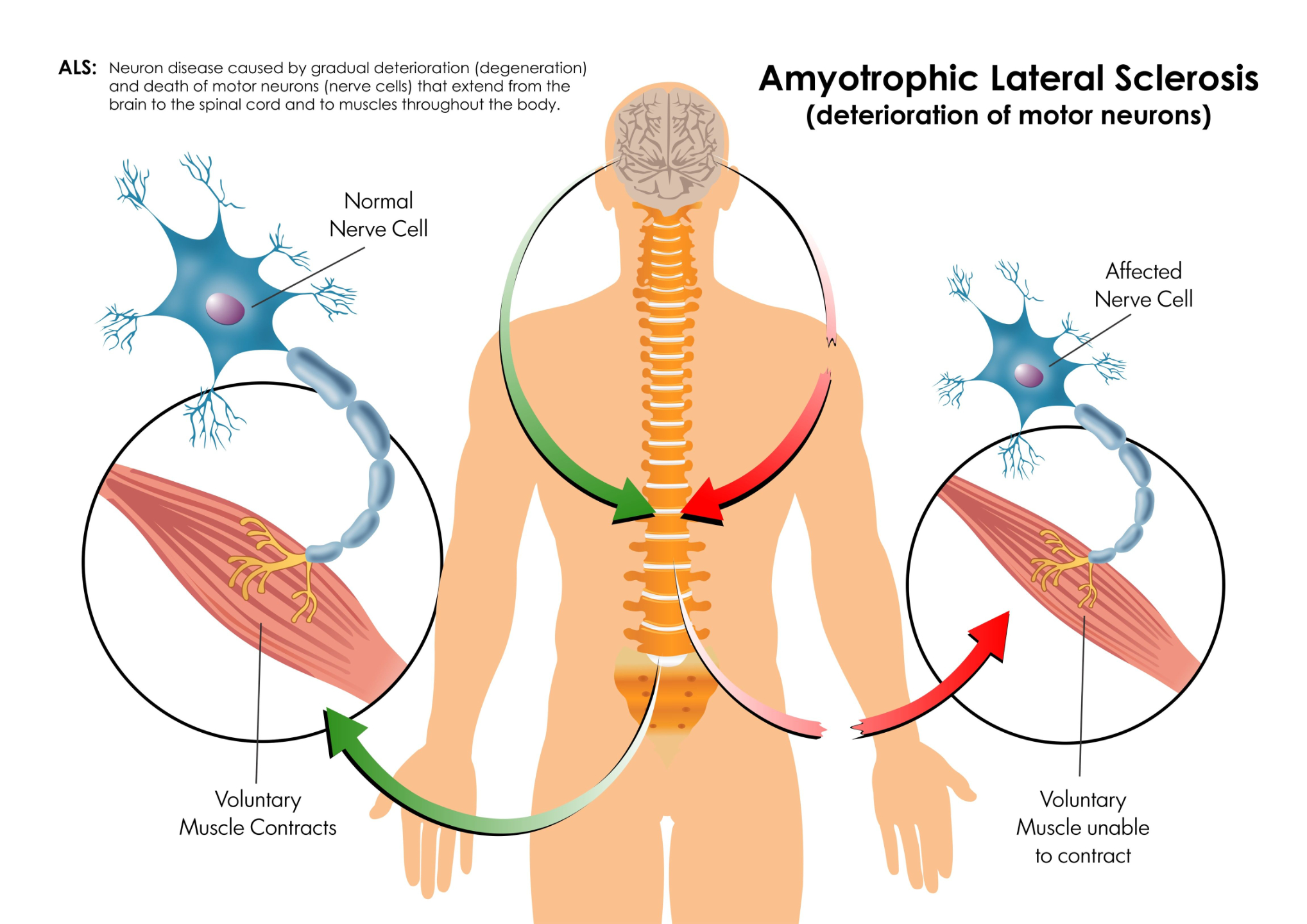
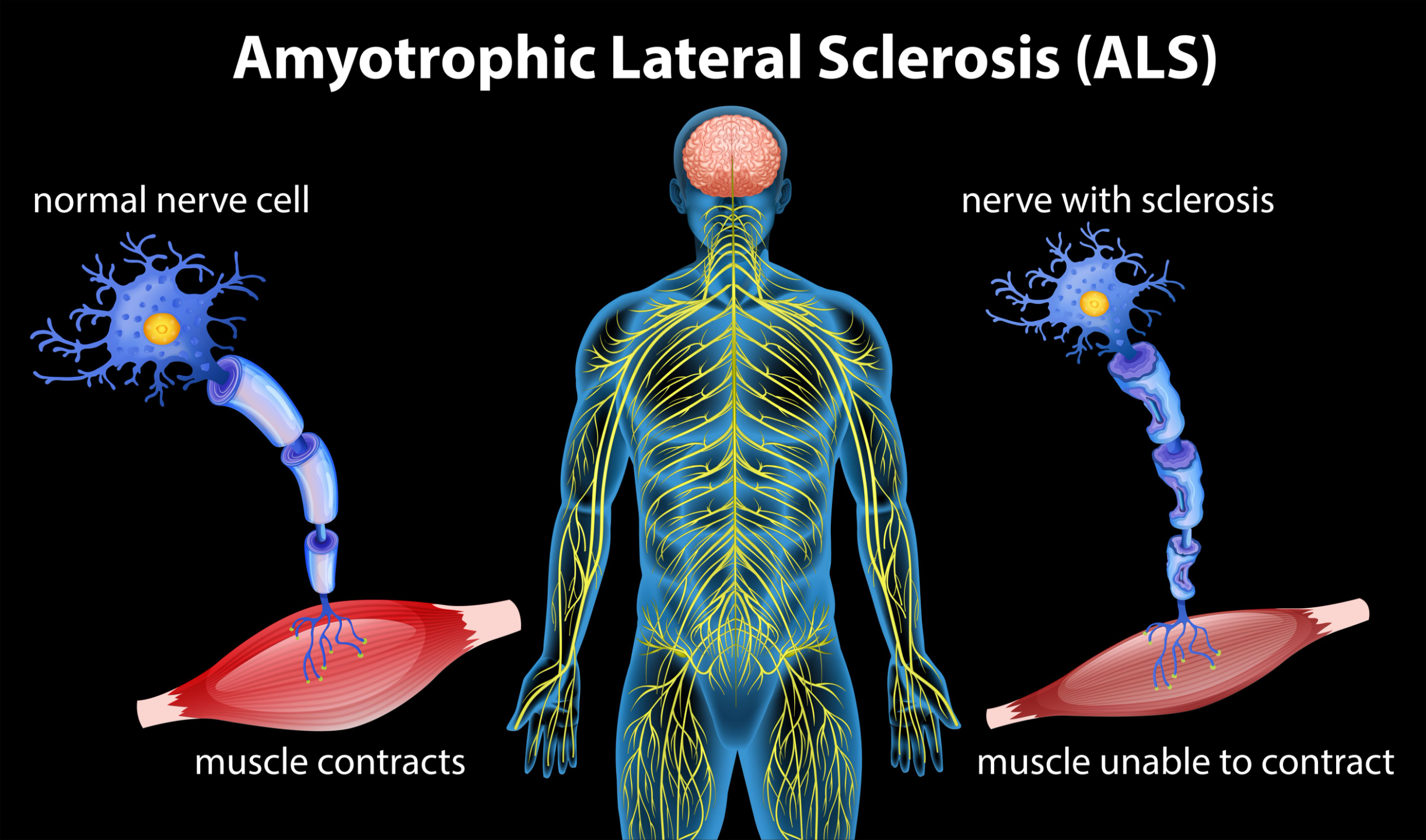
Overview
Lou Gehrig’s disease (professional baseball player died from the dx in 1941)
Most common motor neuron disease with an incidence rate of 2 per 100,000 people
People are usually diagnosed late due to hesitancy in going to neurologist
Men are affected more than women (A story of a woman with ALS)
Cause unknown (combination of genetic, viral, retroviral, autoimmune, neurotoxic factors)
Print General Information about ALS
The "Subjective"
This information is collected from interviews with the patient, as well as input from their professional and social support systems.

The "Objective"
This information is captured using objective Assessments and questionnaires. It is how you determine if you are making progress with your patient.

The "Assessment"
Use your clinical reasoning and evidence-based knowledge to interpret patient data and justify the need for OT services.

The "Plan"
Watch this 15-minute video on treatment planning for tips that apply to this process, regardless of diagnosis.
Evaluation Interview Questions
The interview is your chance to build rapport, answer questions, and gather meaningful information about your patient. Be prepared—don’t wing it. Time is valuable. Download this ready-to-use interview guide to streamline your evaluation.
Download an Interview for ALS
Symptoms & Other Impacts
Symptoms affect quality of life. We don’t treat symptoms directly, but we must acknowledge and talk about them to help clients manage them.
Three types of ALS
(labeled for which symptom it impacts first)
Primary Lateral Sclerosis (slower progression)
Progressive Muscular Atrophy (PMA)
Bulbar Palsy or Bulbar Predominant ALS

Long-term Life Effect
As ALS progresses, it affects nearly every area of daily living. OT practitioners play a vital role in helping clients adapt to these changes while preserving dignity, autonomy, and quality of life.
Download ALS Guide (External Link)

🔄 Functional Decline
-
Muscle weakness and atrophy → Loss of fine motor and gross motor function
-
Decreased endurance → Fatigue during basic tasks like grooming or feeding
-
Reduced mobility → Difficulty with transfers, walking, and eventually bed mobility
🧠 Cognitive and Emotional Considerations
-
Cognitive changes may occur in some ALS types (especially ALS-FTD overlap)
-
Emotional lability (laughing or crying unpredictably)
-
Anxiety, depression, and grief about loss of function
🫁 Respiratory Decline
-
Weakening of respiratory muscles affects:
-
Speech
-
Breathing during sleep
-
Swallowing (aspiration risk)
-
Eventually, respiratory failure
-
🗣️ Speech and Swallowing
-
Dysarthria (slurred speech)
-
Dysphagia (difficulty swallowing)
-
Transition to AAC (augmentative & alternative communication) and PEG feeding may be necessary
🏠 Environmental Needs
-
Progressive need for:
-
Home modifications
-
Transfer aids
-
Power mobility devices
-
Caregiver support
-
🧑🤝🧑 Caregiver Burden
-
Functional changes directly impact caregivers’ mental and physical health
-
OT can support caregiver routines, training, and emotional regulation
Interventions
Clinicians use knowledge, experience, research, judgment, and client input to guide effective interventions.
Build a Holistic Treatment Plan
Occupational therapy plays a vital role in supporting individuals with ALS as they navigate progressive changes in mobility, communication, and daily function. Use the categories below to explore targeted interventions that address both physical decline and quality of life—each rooted in clinical reasoning, adaptability, and client-centered care.
